Background: Idiopathic hypereosinophilia and hypereosinophilic syndrome (HES) comprise a rare, heterogeneous group of hematologic disorders characterized by the overproduction of eosinophils leading to tissue eosinophilic infiltration and damage. Hypereosinophilia can be primary - due to a clonal or malignant process - or secondary to a non-clonal process. Primary eosinophilia can be accompanied by clonal markers, such as in myeloid/lymphoid neoplasms with eosinophilia and rearrangement of PDGFRA/B, FGFR1 or PCM1-JAK2, genetic mutations or chromosomal abnormalities leading to a diagnosis of chronic eosinophilic leukemia. Without easily identifiable clonal markers, a diagnosis of idiopathic HES is made after secondary causes are excluded.
Thrombotic complications in clonal eosinophilic disorders have been described in case reports but the prevalence of thrombosis has not been extensively studied. We hypothesized that HES is associated with an increased thrombotic risk compared to the general population. Additionally, given the known increased thrombotic risk in patients with clonal hematopoiesis of indeterminate potential, we also hypothesized that the risk of thrombosis is greatest in HES patients with evidence of an underlying clonal process.
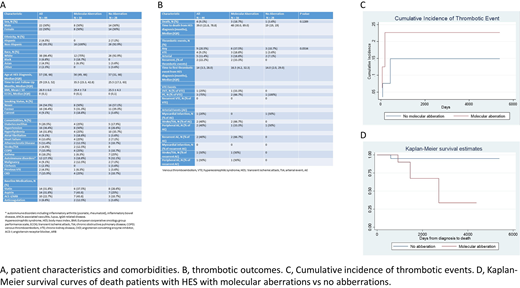
Methods: Using an institutional database, we retrospectively analyzed 44 patients with HES who had undergone molecular testing with a DNA based next generation sequencing (NGS) assay (Heme SnapShot) and an RNA based NGS assay (Heme fusion) as part of their work up for HES at Massachusetts General Hospital from 2016 to 2020. Patients with secondary eosinophilia were excluded. We used Fisher's exact test to compare rates of thrombotic events or death between patients with and without molecular aberration. Relative risk and corresponding 95% CI was estimated by fitting a log-binomial regression model.
Results: Among the 44 patients analyzed, 16 (36.4%) had a molecular aberration detected on NGS. Of the patients with molecular aberrations detected, 4 (25%) had PGFRA, PGFRB, or FGFR1 fusions. Other pathogenic mutations were as follows - 1 (6.3%) JAK2 mutation, 3 (18.8%) TET2, 1 (6.3%) DNMT3A and 9 (56.4%) had mutations in other genes. White blood cell count, absolute eosinophil count, hematocrit, platelet count, tryptase and vitamin B12 levels at diagnosis of HES were similar between the two groups. After a median follow-up time of 29 months (IQR 19.3, 52), 9 (20.5%) of all HES patients had a thrombotic event after diagnosis of HES (4 venous and 5 arterial) with a median time to first thrombotic event of 14.0 months (IQR 3.5, 28.0). HES patients with a molecular aberration had increased number of thrombotic events compared to HES patients with no molecular aberrations, 37.5% versus 10.7% respectively (p = 0.053, risk ratio 3.5, 95% CI 1.01 - 12.12). Three patients with molecular aberrations died versus 1 patient with no molecular aberrations (p = 0.129, risk ratio 5.25, 95% CI 0.59 - 46.36). Among patients with at least 12 months of follow-up (n = 40, 14 with and 26 without molecular aberrations), the one-year cumulative incidence of thrombotic events was 42.9% in patients with molecular aberrations vs 11.5% without (p = 0.044, RR 3.7 95% CI 1.2-12.0). HES patients who had thrombotic events had an increased risk of death compared to those without thrombotic events (p = 0.0226, RR 11.7, 95% CI 1.8 - 75.2).
Conclusions: Thrombotic complications are common in the current study of patients with HES and are associated with an increased risk of death. Although our patient cohort was small, presence of molecular aberrations had increased rates of thrombotic events and mortality, suggesting an area of further study including possible therapeutic trials.
Brunner:Takeda: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; AstraZeneca: Research Funding; Forty-Seven Inc: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Al-Samkari:Argenx: Consultancy; Amgen: Research Funding; Dova: Consultancy, Research Funding; Agios: Consultancy, Research Funding; Rigel: Consultancy. Rosovsky:Bristol-Myers Squibb, Janssen: Research Funding; Bristol-Myers Squibb, Dova, Janssen, Portola: Consultancy. Fathi:PTC Therapeutics: Consultancy; Takeda: Consultancy; TrovaGene: Consultancy; Amgen: Consultancy; Bristol-Myers Squibb: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Astellas: Consultancy; Novartis: Consultancy; NewLink Genetics: Consultancy, Honoraria; Daiichi Sankyo: Consultancy; Forty Seven: Consultancy; Jazz: Consultancy, Honoraria; Kite: Consultancy, Honoraria; Trillium: Consultancy; Seattle Genetics: Consultancy, Research Funding; Pfizer: Consultancy; Kura: Consultancy; Boston Biomedical: Consultancy; Blue Print Oncology: Consultancy; AbbVie: Consultancy; Agios: Consultancy, Research Funding; Amphivena: Consultancy, Honoraria. Weitzman:Abbvie: Consultancy. Hobbs:Incyte: Research Funding; Bayer: Research Funding; Novartis: Honoraria; Celgene/BMS: Honoraria; Merck: Research Funding; Constellation: Honoraria, Research Funding; Jazz: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.